Weakley County STDs on the Rise
Shannon Taylor
Editor
Weakley County saw an increase in sexually transmitted infections since 2000 according to a recently released 2022 report from the Centers of Disease Control (CDC).
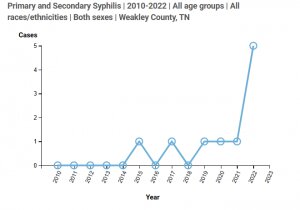
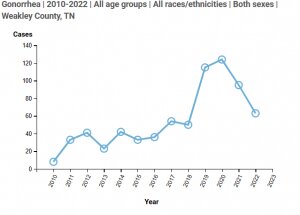
Chlamydia rates have more than doubled since 2000, while gonorrhea more than tripled over the same period. The Centers for Disease Control and Prevention report showed that syphilis rates are now reaching the same levels seen in the 1950s.
Counties in Tennessee are ranked by the CDC according to the rate of infections with chlamydia being the most prominent STI nationally.
State-level statistics show Chlamydia cases at 538.1 per 100K in Tennessee. Tennessee is #12 nationally for chlamydia cases with 37,942 cases reported in 2022. Gonorrhea cases were at 227.9 per 100K with Tennessee being #11 nationally with 16,069 cases reported in 2022. Primary and secondary syphilis cases were at 16 per 100K with Tennessee being #23 nationally with 1,126 cases reported in 2022.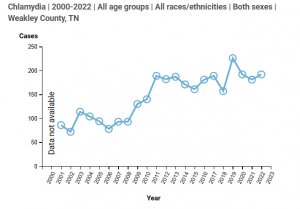
Weakley came in at #13 across the state for the highest rates of STI’s reported. Chlamydia cases were at 547.9 per 100K with 181 cases reported in Weakley County in 2022. In 2001 only 86 cases were reported. Gonorrhea cases were at 287.6 per 100K with 95 cases reported in 2022. In 2010 only 8 cases were reported. Syphilis cases were at 9.1 per 100K with 3 cases reported in 2022. In 2010 there were 0 cases reported.
Other counties in Tennessee also reported higher cases than previous years.
Shelby County came in at the #1 spot with 9,902 cases of chlamydia reported in 2022 making the county have 1,071 per 100K people. Shelby’s data showed gonorrhea cases at 5,192 with 561.6 per 100K people and syphilis cases at 680 with 73.6 per 100K people.
Obion County came in at #17. Obion County reported 164 cases of chlamydia in 2022 with 538.3 per 100K people, 110 cases of gonorrhea with 361.1 per 100K people and only 1 case of syphilis during the 2022 reporting year.
It’s important to note that ‘duty to warn’ is a legal concept that indicates possibly liability for healthcare providers if no warning of possible harm is given in certain circumstances, according to the CDC, however, a direct “duty to warn” third parties that they may need a medical examination because of their potential STD exposure was not found across states, despite its existence for other serious medical conditions.
A duty to warn health law exists due to findings from a widely referenced case: Tarasoff v. Regents of the University of California, in which a court found that a psychologist should have warned his patient’s girlfriend after his patient told the psychologist of his intention to kill her, despite the competing consideration of physician/patient confidentiality.
In the area of health law, “duty to warn” describes a physician’s responsibility to warn an identifiable third party of a potential serious threat of harm to their health.
The only action that physicians are required to take beyond diagnosis and treatment of their patient is reporting the case to the state or local health department, per the laws of their state. Physician duties generally do not extend to sex partners of diagnosed patients, and as a result, sex partners are not always notified. Some states may require additional reporting of “suspected cases,” which can include partners of diagnosed patients, according to the CDC.
According to the CDC, many state health departments, however, often use partner notification and contact tracing — two integral components of partner services — to break the chain of STD transmission because these strategies can help pinpoint the window of possible infection. They are most often used when syphilis is the STD in question because of the serious, long-term health risks associated with non-treatment. Limited partner notification services for other STDs (e.g., gonorrhea and chlamydia) may be conducted based on health department resources. Health departments also can encourage patients to notify their partners or provide patients with medication for their partners—a practice known as expedited partner therapy (EPT). All patients diagnosed with an STD are covered by patient confidentiality, and specially trained health department staff conduct contact tracing and partner notification while maintaining confidentiality. These activities are widely seen as effective in reducing the STD burden in communities and are supported by CDC.
For the prevention of STI’s the CDC recommends abstinence as the most reliable way, vaccines for HPV and Hepatitis B, reducing the number of sexual partners, mutual monogamy (agreeing to be sexually active with only one person), and using condoms every time you have sexual intercourse.
STI’s impact the health of millions in the United States each year. The reported number of STI’s has been on the rise since 1014 with no sign of slowing down, according to the CDC. Infections also disproportionately affect those under the age of 25, racial and ethnic minority groups, and gay or bisexual men, according to CDC data.
The CDC warns that STI’s can have serious health consequence and that people don’t always experience symptoms, however, if left untreated it can increase the chance for HIV infection, chronic pelvic pain, pelvic inflammatory disease, infertility, severe pregnancy and newborn complications and infant death.
If you’re sexually active, it is important to schedule regular check-ups to be tested with your primary care physician or local health department.





